Abstract

Introduction
Incidentally noted mild thrombocytopenia (platelet count of 100-150 K/uL) in otherwise healthy individuals is a frequent reason for hematology referrals. Most of these patients are asymptomatic and have had this laboratory finding for a considerable number of years prior to the referral. In addition, an extensive workup is usually ordered in an attempt to find an underlying pathology. We conducted this study to assess the utility of hematology referrals and workup carried for patients with mild thrombocytopenia as a step towards a standardized approach and evidence-based referral and testing algorithms.
Methods
We searched for outpatient hematology referrals with a diagnosis of thrombocytopenia using ICD-9 and ICD-10 diagnostic codes at Henry Ford Health System (Detroit, MI) database between June 2013 and June 2016. Data collected included patient demographics, platelet count, clinical symptoms and any workup carried for thrombocytopenia at the time of presentation. The development of any of the following outcomes was observed for a period of 1 year from their initial visit: hematological malignancy, rheumatologic disorder, infectious disease or bleeding. Only patients with mild thrombocytopenia at the time of referral were included. Patients were excluded if they had any of the following: moderate or severe thrombocytopenia (platelet count less than 100 K/uL or less than 50 K/uL respectively), known hematological disorder or malignancy, on active chemotherapy or if seen before by a hematologist for a platelet-related disorder.
Results
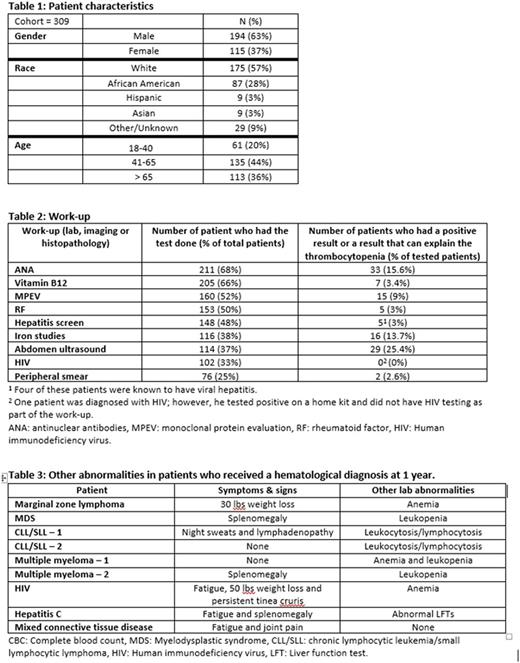
A total of 580 patients were seen in our hematology clinics during the study period with a diagnostic code for thrombocytopenia, of which 271 were excluded (137 had moderate thrombocytopenia, 36 had severe thrombocytopenia and 98 were excluded based on one or more of the criteria above). The remaining 309 patients (53%) had mild thrombocytopenia and constituted our cohort. Patient characteristics are shown in table 1.
Initial workup ranged from repeating a complete blood count to a battery of tests aimed at finding an underlying pathology. The most commonly ordered tests with the percentage of positive results are shown in table 2.
At the 1 year follow-up mark, 6 patients (1.9%) were diagnosed with a hematological malignancy (marginal zone lymphoma with plasmacytic differentiation; n=1, myelodysplastic syndrome; n=1, chronic lymphocytic leukemia/small lymphocytic lymphoma; n=2 and Multiple Myeloma; n=2), 2 patients (0.6%) were diagnosed with an infectious disease (Human immunodeficiency virus; n=1 and hepatitis C; n=1) and only 1 patient (0.3%) had a new rheumatologic diagnosis (mixed connective tissue disease). Most importantly, these 9 patients had other symptoms, signs, abnormal labs or imaging studies beside the mild thrombocytopenia that warranted further workup at time of initial evaluation (table 3). None of the remaining 300 patients developed any significant clinical condition at 1 year.
Conclusion:
Hematology referrals for isolated mild thrombocytopenia are a very frequent reason for hematology clinic visits with a very low yield of such an evaluation. This study shows that in patients who are asymptomatic and without other abnormalities on complete blood count, workup did not reveal any hematological, infectious or rheumatologic diagnoses. In addition, this study demonstrates the need for an algorithmic approach for referring physicians and primary care providers to identify patients who might need a more extensive evaluation to maximize the benefit gained from hematology referrals.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract